The Laboratory Meets Level Ii Biosafety Standards
Explain some terms:
Laboratory biosecurity: is the term used to describe the principles, techniques and practices necessary to prevent unwanted exposure or loss of pathogens and toxin.
Decontamination is the process of eliminating and destroying bacteria. Eliminate or neutralize hazardous substances and radioactive substances. The decontamination process including cleaning, disinfection and sterilization is carried out depending on the safety and practical requirements of each laboratory.
Cleaning: is the process of using water, brush, mop, sweep, and cleaning chemicals to remove all dirt, rubbish and scattered chemicals
Sterilization: is the process of eliminating virtually all pathogenic microorganisms except bacterial spores.
Sterilization: is the process of eliminating nearly all the pathogenic microorganisms including their spores.
Laboratory employees: including all people working in laboratories such as the persons in charge of the laboratories, the testers or decontamination workers
Purpose of biosafety laboratory:
Protect the technician and all laboratory staff
Protecting specimens, not cross-contaminating all other agents.
Protect people outside the laboratory and the surrounding environment.
 .
.Conditions for a laboratory to achieve biosafety level II
Conditions on facilities:
The floors, walls, and test tables must be flat, impermeable, heat resistant and corrosive and easy to clean.
There is a hand wash sink, and an eyewash emergency, first aid box.
There is electricity along with the grounding system and there is a backup power source.
There is clean water, and the water supply pipeline directly to the testing area must have anti-backflow devices to protect the public water system.
Having full equipment for fire and explosion prevention and fighting
There is enough light to perform the test
There is a system for collecting and treating wastewater treatment equipment. Testing establishments operating before the effective date of this Decree are required to have results of waste water testing meeting national technical standards on environment before discharging them into shared wastewater reservoirs.
Must be set separately from other rooms of the testing facility.
There is a biohazard sign on the entrance and testing area.
 .
.Conditions on operating equipment:
The testing equipment must conform to the technique and specimen or microorganism tested.
Have the prescribed packaging, tools, and equipment for storing medical waste.
There are equipment to disinfect tools as well as specimens.
Biosafety cabinets are required
There are steaming equipment for infectious medical waste or disinfection equipment
Personal protective equipment suitable for each type of testing technique performed at the biosafety level II biosafety testing facility
Personnel conditions:
Number of employees: At least 02 testing staff. Personnel directly performing microbiological tests (hereinafter referred to as testing staff for short) must possess diplomas and certificates of training suitable to the type of testing conducted by that establishment.
Establishments with laboratories must assign persons responsible for biosafety.
Testing personnel and persons responsible for biosafety must be adequately trained in biosafety from level II or higher.
Others working in the laboratory area must be instructed on biosafety appropriate to the job.
Conditions for practice:
There are rules for entry and exit of the laboratory area.
 .
.There are regulations on reporting regime.
There is a procedure for record keeping
There is an appropriate testing procedure and the sample or microorganisms are tested.
There are instructions on the use of equipment for testing activities;
There is a procedure for decontamination and medical waste treatment.
There are rules for health and medical supervision.
There is a plan for training and staff training in the testing area.
There are regulations for storage and storage of specimens and infectious pathogens at the testing facility.
There is a plan to assess the risk of possible biosafety incidents at the laboratory and develop a prevention plan, as well as handle biosafety incidents.
KTV. KHONG VY.
 . Dịch vụ: Thiết kế website, quảng cáo google, đăng ký website bộ công thương uy tín
. Dịch vụ: Thiết kế website, quảng cáo google, đăng ký website bộ công thương uy tínRelated news
-
 Parasitical Worms.com Tests to find the cause of urticaria, diagnosis of urticaria results will be available throughout the day. After the results the doctor will explain, point out the abnormal signs for your child to understand and he will prescribe medication for home. Question Hello doctor: I ...
Parasitical Worms.com Tests to find the cause of urticaria, diagnosis of urticaria results will be available throughout the day. After the results the doctor will explain, point out the abnormal signs for your child to understand and he will prescribe medication for home. Question Hello doctor: I ... Parasitical Worms.com Adult flukes are very small, 3 - 6 mm long, with 4 suction heads and a double hook, very short neck; coal consists of 3 segments, the final flukes have several hundred eggs, size 45 x 35 mcm, very similar to Toenia spp eggs. The disease is caused by the larva Echinococcus ...
Parasitical Worms.com Adult flukes are very small, 3 - 6 mm long, with 4 suction heads and a double hook, very short neck; coal consists of 3 segments, the final flukes have several hundred eggs, size 45 x 35 mcm, very similar to Toenia spp eggs. The disease is caused by the larva Echinococcus ... Parasitical Worms.com Some diseases caused by larvae of the anisakinae family parasitize marine mammals. In humans, the parasite falls into a dead-end, or severe or severe illness depending on the place of parasite, number of larvae and tissue responses. Diagnosis is often difficult and the most ...
Parasitical Worms.com Some diseases caused by larvae of the anisakinae family parasitize marine mammals. In humans, the parasite falls into a dead-end, or severe or severe illness depending on the place of parasite, number of larvae and tissue responses. Diagnosis is often difficult and the most ... Parasitical Worms.com Illness caused by the nematode of Angiostrongylus cantonensis parasitizes and causes disease in the meninges, invasion of the brain can lead to death. Commonly called Meningitis - brain caused by Angiostrongylus cantonensis. The causative agent of nematode ...
Parasitical Worms.com Illness caused by the nematode of Angiostrongylus cantonensis parasitizes and causes disease in the meninges, invasion of the brain can lead to death. Commonly called Meningitis - brain caused by Angiostrongylus cantonensis. The causative agent of nematode ... Fascioliasis is two types of fascioliasis and small liver fluke. People are infected with food, skin. Flukes can cause hepatitis, liver tumors, liver necrosis, but fortunately, liver fluke can be cured if detected early, treated in a reputable facility with a good doctor, using drugs. Good, ...
Fascioliasis is two types of fascioliasis and small liver fluke. People are infected with food, skin. Flukes can cause hepatitis, liver tumors, liver necrosis, but fortunately, liver fluke can be cured if detected early, treated in a reputable facility with a good doctor, using drugs. Good, ... Parasitical Worms.com Diagnosis is determined by seeing sparganum larvae from the wound. Clinical and prehistoric images of frog meat, eye-copying as well as the habit of eating undercooked snakes, mice, and eels are important factors for diagnosis. Doctor: Le Thi Huong Giang Medical Consultation: ...
Parasitical Worms.com Diagnosis is determined by seeing sparganum larvae from the wound. Clinical and prehistoric images of frog meat, eye-copying as well as the habit of eating undercooked snakes, mice, and eels are important factors for diagnosis. Doctor: Le Thi Huong Giang Medical Consultation: ... MUSHROOM DISEASE (Aspergillus) 1. Epidemiology. Aspergillus fungus is one of the largest fungal strains, present in all over the world, there are about 100 species, currently there are about 20-30 species that cause disease in humans, important strains are A. fumigatus, A. flavus , A. niger such as ...
MUSHROOM DISEASE (Aspergillus) 1. Epidemiology. Aspergillus fungus is one of the largest fungal strains, present in all over the world, there are about 100 species, currently there are about 20-30 species that cause disease in humans, important strains are A. fumigatus, A. flavus , A. niger such as ... MUSHROOM DISEASE Cryptococcosis (Tolurosis, European Blastomycois) 1. Etiology and epidemiology Cryptococcosis is also known as the European Blastomycose mycosis caused by Cryptoccocus neoformans, a thick cystic yeast, has serotypes A, D (C. neoformans var. Neoformans) and B, C ( C.neoformans var. ...
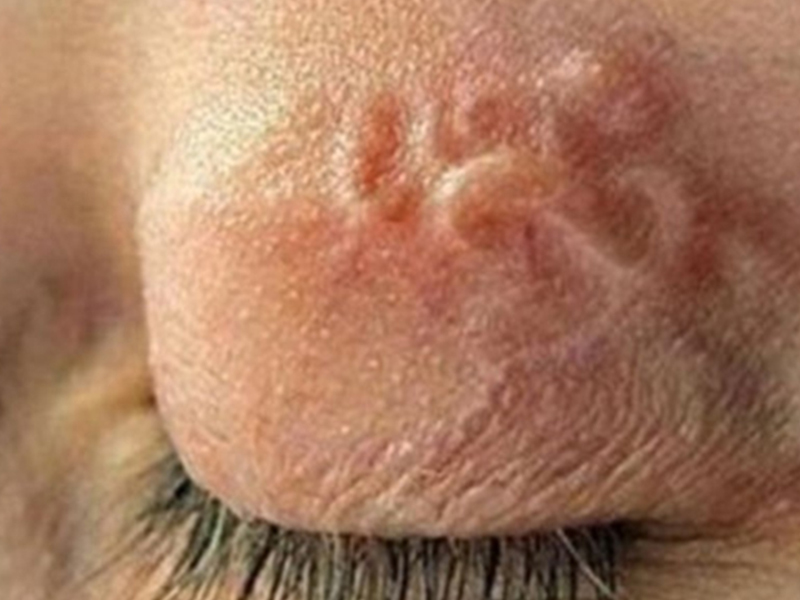
MUSHROOM DISEASE Cryptococcosis (Tolurosis, European Blastomycois) 1. Etiology and epidemiology Cryptococcosis is also known as the European Blastomycose mycosis caused by Cryptoccocus neoformans, a thick cystic yeast, has serotypes A, D (C. neoformans var. Neoformans) and B, C ( C.neoformans var. ... MUSHROOM DISEASE Sporotrichosis (Gardener Disease) 1. Epidemiology and etiology Sporotrichosis is a chronic disease caused by Sporothrix schenckii that causes damage to the skin or internal organs (also known as gardener disease - gardener's disease). This is a dimorphic mushroom. In nature, ...
MUSHROOM DISEASE Sporotrichosis (Gardener Disease) 1. Epidemiology and etiology Sporotrichosis is a chronic disease caused by Sporothrix schenckii that causes damage to the skin or internal organs (also known as gardener disease - gardener's disease). This is a dimorphic mushroom. In nature, ... CANDIDA MUSHROOM 1. Germs Candidiasis is an acute, subacute or chronic disease caused by Candida-like yeasts, mostly Candida albicans. Candidiasis is available in the body (bronchus, oral cavity, intestine, vagina, skin around the anus) normally in non-pathogenic form. When having favorable ...
CANDIDA MUSHROOM 1. Germs Candidiasis is an acute, subacute or chronic disease caused by Candida-like yeasts, mostly Candida albicans. Candidiasis is available in the body (bronchus, oral cavity, intestine, vagina, skin around the anus) normally in non-pathogenic form. When having favorable ...