How Is It Treated?
Parasitical Worms.com The small active form (Entamoeba histolytica forma minuta) lives in the colon with a size of 8-25 micrometers, moving slower than the large active body, in the cytosol without red blood cells.
Define
Amoeba is Entamoeba histolytica protozoan infection, a disease characterized by ulcers in the lining of the colon and capable of causing abscesses in different organs (liver, brain ..
Research history
In 1875, F A. Lesch first discovered the amoeba in the stool of a dysentery patient in Peterburg.
 . He has caused experimental amoebic dysentery for 4 dogs. On the eighteenth day of his illness, he slaughtered a dog and looked at the colon for a lot of ulcers.
. He has caused experimental amoebic dysentery for 4 dogs. On the eighteenth day of his illness, he slaughtered a dog and looked at the colon for a lot of ulcers.In 1883, R. Koch studied the anatomy of dysentery dysentery in Egypt. He found amoeba on slices through the ulcer, through the walls of the liver abscess in 4 corpses
In 1891 Councilman and Lafleur named the disease and called it 'amoebic dysentery'
In 1903 Shaudin identified the single cell of the Entamoebidae family and called it Entamoeba histolytica. They have two forms: the active and non-pathogenic activity.
In 1904 Kartulis found amoeba in the brain abscess.
In 1912, Emetin was started to treat amoeba.
 .
.Epidemiology and pathogen
Epidemiology: Entamoeba histolytica protozoan belongs to Entamoebidae family, Amoebida order, Protozoa branch. The life cycle of a divided amoeba is 2 periods: The period of activity and the period of rest (cocoon). However, it can change from active to resting or vice versa depending on the nutritional conditions of the host's environment. Based on the appearance and physiology of E histolytica, it is divided into 3 types of dysentery:
The large active form (Entamoeba histolytica forma magna) is collected in the feces, the mucous-blooded area of patients with intestinal amoeba, size 15-30 micrometres, is most active at 37 ° C and pH 6.5. In the cytoplasm of amoeba has many red blood cells. E. histolytica forma magna enters cells, usually contracting in the cytoplasm with a size of 4-8 micrometers.
The small active form (Entamoeba histolytica forma minuta) lives in the colon with size ranging from 8-25 micrometers slower than the large active body, in the cytoplasm without red blood cells.
 .
.Cocoon (Entamoeba histolytica forma cystica) is a form of small active form. Cocoons are oval or round in diameter from 10-14 micrometres, surrounded by 2 shells The young cocoon has 1 core but when old it has 4. Cocoon formation is indispensable in the amoeba life cycle and plays a role in disease transmission.
Inoculum
Patients (both acute and chronic) and healthy people carry amoeba cysts that contaminate food and drinking water. Some animals, such as monkeys, dogs, cats, rats etc. can get sick but they do not pick up cocoons so they are not a source of disease.
Pathogen: Transmitted via gastrointestinal tract due to food, drinking water contaminated with amoeba. Amoeba cocoons exist relatively well in the outside: at 17-20 ° C they exist for months; at 45 ° C the cocoon dies after 30 minutes, at 85 ° C dies after a few seconds. With Crezyl 1/250 disinfectant can kill cocoon cocoon within 5-15 minutes.

Body receptor - immune
All ages can catch amoeba, but 90% of people infected have no symptoms, only 10% of infected people have symptoms of amoebic dysentery or abscesses in different organs.
People infected with E. histolytica will form local immunity (in the intestinal wall) and the whole body but will not have a firm protection against invading pathogens.
Translation properties
The disease usually spreads. However, in tropical countries with low economic and social life, diseases can cause major epidemics.
Pathogenesis and pathological mechanisms
Cocoon amoeba through food, drinking water .. enters the human body through the digestive tract. Upon reaching the stomach, thanks to the effect of the gastric juice, the four shells in the cocoon are released and develop into 4 small amoeba (forma minuta) then they move down to reside in the ileum which is rich in nutrients.
 . , pH is appropriate and there are many symbiotic bacteria. Normally, small amoeba does not penetrate into the intestinal wall to cause disease but is excreted in the stool in the colon. Some small amoeba shrink into cocoons and also excreted in the faeces as a risk of spreading to others.
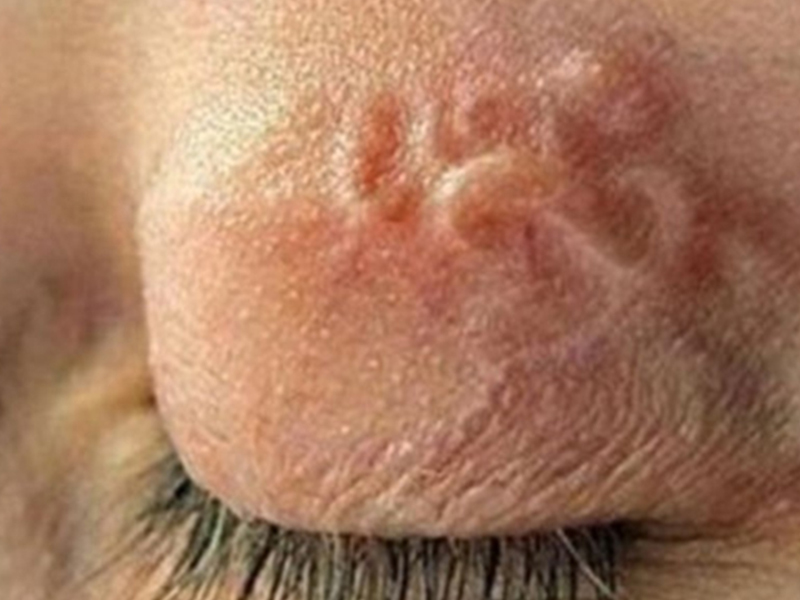
. , pH is appropriate and there are many symbiotic bacteria. Normally, small amoeba does not penetrate into the intestinal wall to cause disease but is excreted in the stool in the colon. Some small amoeba shrink into cocoons and also excreted in the faeces as a risk of spreading to others.When the intestinal wall is injured (by another bacteria or injury), the small amoeba can enter the intestinal wall, reproduce there and secrete protein-digesting enzymes that lead to necrotizing intestinal cell necrosis. At the intestinal wall, the amoeba initially causes congestion in the mucosa, then forms small lumps on the mucous surface of the mucosa, which eventually becomes necrotic and ulcerative. The sores can be up to 2-25cm wide, around the edge of the erection, edema and congestion. The bottom of the ulcer deepens to the submucosa and is covered with pus. The ulcers that are close together can communicate with each other to form a larger ulcer, deeper into the muscle layer and together with the bacteria that form deep abscesses, which can cause intestinal perforation and purulent peritonitis. Amoeba also creates granulomas in the intestinal wall that are sometimes difficult to distinguish from.
 . . Dịch vụ: Thiết kế website, quảng cáo google, đăng ký website bộ công thương uy tín
. . Dịch vụ: Thiết kế website, quảng cáo google, đăng ký website bộ công thương uy tínRelated news
-
 Parasitical Worms.com Tests to find the cause of urticaria, diagnosis of urticaria results will be available throughout the day. After the results the doctor will explain, point out the abnormal signs for your child to understand and he will prescribe medication for home. Question Hello doctor: I ...
Parasitical Worms.com Tests to find the cause of urticaria, diagnosis of urticaria results will be available throughout the day. After the results the doctor will explain, point out the abnormal signs for your child to understand and he will prescribe medication for home. Question Hello doctor: I ... Parasitical Worms.com Adult flukes are very small, 3 - 6 mm long, with 4 suction heads and a double hook, very short neck; coal consists of 3 segments, the final flukes have several hundred eggs, size 45 x 35 mcm, very similar to Toenia spp eggs. The disease is caused by the larva Echinococcus ...
Parasitical Worms.com Adult flukes are very small, 3 - 6 mm long, with 4 suction heads and a double hook, very short neck; coal consists of 3 segments, the final flukes have several hundred eggs, size 45 x 35 mcm, very similar to Toenia spp eggs. The disease is caused by the larva Echinococcus ... Parasitical Worms.com Some diseases caused by larvae of the anisakinae family parasitize marine mammals. In humans, the parasite falls into a dead-end, or severe or severe illness depending on the place of parasite, number of larvae and tissue responses. Diagnosis is often difficult and the most ...
Parasitical Worms.com Some diseases caused by larvae of the anisakinae family parasitize marine mammals. In humans, the parasite falls into a dead-end, or severe or severe illness depending on the place of parasite, number of larvae and tissue responses. Diagnosis is often difficult and the most ... Parasitical Worms.com Illness caused by the nematode of Angiostrongylus cantonensis parasitizes and causes disease in the meninges, invasion of the brain can lead to death. Commonly called Meningitis - brain caused by Angiostrongylus cantonensis. The causative agent of nematode ...
Parasitical Worms.com Illness caused by the nematode of Angiostrongylus cantonensis parasitizes and causes disease in the meninges, invasion of the brain can lead to death. Commonly called Meningitis - brain caused by Angiostrongylus cantonensis. The causative agent of nematode ... Fascioliasis is two types of fascioliasis and small liver fluke. People are infected with food, skin. Flukes can cause hepatitis, liver tumors, liver necrosis, but fortunately, liver fluke can be cured if detected early, treated in a reputable facility with a good doctor, using drugs. Good, ...
Fascioliasis is two types of fascioliasis and small liver fluke. People are infected with food, skin. Flukes can cause hepatitis, liver tumors, liver necrosis, but fortunately, liver fluke can be cured if detected early, treated in a reputable facility with a good doctor, using drugs. Good, ... Parasitical Worms.com Diagnosis is determined by seeing sparganum larvae from the wound. Clinical and prehistoric images of frog meat, eye-copying as well as the habit of eating undercooked snakes, mice, and eels are important factors for diagnosis. Doctor: Le Thi Huong Giang Medical Consultation: ...
Parasitical Worms.com Diagnosis is determined by seeing sparganum larvae from the wound. Clinical and prehistoric images of frog meat, eye-copying as well as the habit of eating undercooked snakes, mice, and eels are important factors for diagnosis. Doctor: Le Thi Huong Giang Medical Consultation: ... MUSHROOM DISEASE (Aspergillus) 1. Epidemiology. Aspergillus fungus is one of the largest fungal strains, present in all over the world, there are about 100 species, currently there are about 20-30 species that cause disease in humans, important strains are A. fumigatus, A. flavus , A. niger such as ...
MUSHROOM DISEASE (Aspergillus) 1. Epidemiology. Aspergillus fungus is one of the largest fungal strains, present in all over the world, there are about 100 species, currently there are about 20-30 species that cause disease in humans, important strains are A. fumigatus, A. flavus , A. niger such as ... MUSHROOM DISEASE Cryptococcosis (Tolurosis, European Blastomycois) 1. Etiology and epidemiology Cryptococcosis is also known as the European Blastomycose mycosis caused by Cryptoccocus neoformans, a thick cystic yeast, has serotypes A, D (C. neoformans var. Neoformans) and B, C ( C.neoformans var. ...
MUSHROOM DISEASE Cryptococcosis (Tolurosis, European Blastomycois) 1. Etiology and epidemiology Cryptococcosis is also known as the European Blastomycose mycosis caused by Cryptoccocus neoformans, a thick cystic yeast, has serotypes A, D (C. neoformans var. Neoformans) and B, C ( C.neoformans var. ... MUSHROOM DISEASE Sporotrichosis (Gardener Disease) 1. Epidemiology and etiology Sporotrichosis is a chronic disease caused by Sporothrix schenckii that causes damage to the skin or internal organs (also known as gardener disease - gardener's disease). This is a dimorphic mushroom. In nature, ...
MUSHROOM DISEASE Sporotrichosis (Gardener Disease) 1. Epidemiology and etiology Sporotrichosis is a chronic disease caused by Sporothrix schenckii that causes damage to the skin or internal organs (also known as gardener disease - gardener's disease). This is a dimorphic mushroom. In nature, ... CANDIDA MUSHROOM 1. Germs Candidiasis is an acute, subacute or chronic disease caused by Candida-like yeasts, mostly Candida albicans. Candidiasis is available in the body (bronchus, oral cavity, intestine, vagina, skin around the anus) normally in non-pathogenic form. When having favorable ...
CANDIDA MUSHROOM 1. Germs Candidiasis is an acute, subacute or chronic disease caused by Candida-like yeasts, mostly Candida albicans. Candidiasis is available in the body (bronchus, oral cavity, intestine, vagina, skin around the anus) normally in non-pathogenic form. When having favorable ...